
Luteinized Unruptured Follicles and NFP Charting
April 4, 2024
Body Positivity for Catholics
April 16, 2024Cervical Ectropion and NFP Charting
This week, let's explore another topic which often befuddles NFP charters:
Cervical Ectropion
The CERVIX is the lower part of the uterus-- what I explain to girls is like the lower neck of a funnel-- which connects the uterus to the vaginal canal. The cervix contains many side chambers, or "crypts" in which fluid/mucus is produced and stored throughout the cycle.
A normal anatomy of the cervix includes interior lining with glandular cells, a transitional zone where the cells change features and then eventually lead to the exterior of the cervix (called the ectocervix) which is covered in harder, more compact squamous cells-- as seen below:
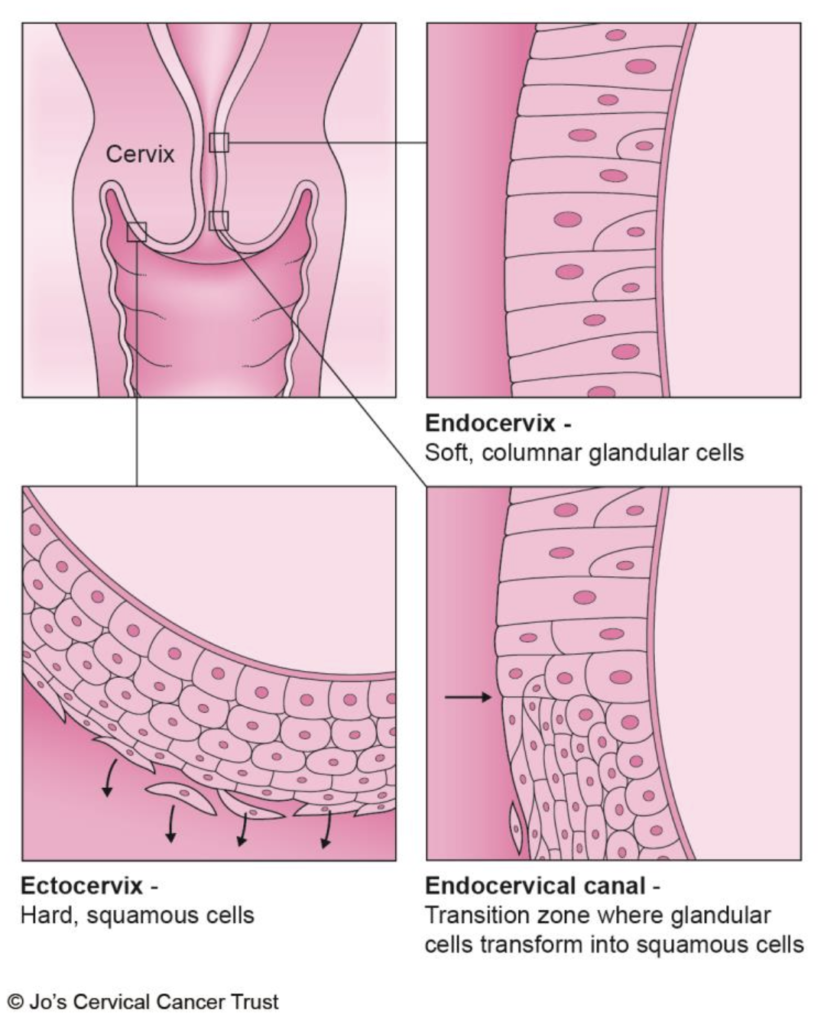
image source: https://www.jostrust.org.uk/sites/default/files/the_cervix_1.2.pdf
When a woman experiences cervical ectropion (also called "cervical erosion") the glandular cells sort of over-produce themselves, and spill outside the inner part of the cervix, where the harder squamous cells should be instead. The effect is a visual reddening of the exterior of the cervix. It is a benign condition, and considered a normal variant to sometimes see.
What causes cervical ectropion?
Cervical ectropion can be thought of in some ways as "hyper stimulation of the cervix," which occurs under the influence of estrogen. There are some women who just naturally don't have as robust of a transitional zone between the glandular and squamous cells and for these women, it may be a persistent and chronic issue. But for the vast majority of women, the condition is considered relatively temporary and is just caused by lots of estrogen working on those cervical cells!
This means that cervical ectropion is more common in times when estrogen is high, including:
- close to ovulation
- adolescence
- certain stages of perimenopause (usually very early stages!)
- when taking synthetic estrogen
- pregnancy
What are the symptoms of cervical ectropion?
Many women won't likely notice any major symptoms with cervical ectropion, altho a doctor may mention noticing the red cells during an exam. If women do experience symptoms, the most likely things to notice would be:
- increased fluid signs, since the glandular cells can produce fluid
- bleeding or pain after intercourse (because of irritation)
- intermenstrual bleeding
- pelvic pain or frequent back ache
- trouble with urination
- inflammation of the cervix
Because many other conditions can produce similar symptoms, it is important to ask your doctor for evaluation if any of these signs are present!
How is cervical ectropion treated? Does it need to be treated?
In many cases, cervical ectropion does not need any particular treatment because the hormonal conditions will change and the ectropion will resolve on its own. If there's an obvious contributor (e.g., taking hormonal contraceptives) then treatment would simply involve removing that particular issue.
But, in some cases, ectropion can interfere with daily life and should be tended to. Some of the more common treatment options are:
- cautery (either by freezing or by electrocautery)
- microwave tissue coagulation
- laser therapy
- boric acid suppositories
How could cervical ectropion impact my charts?
I briefly contributed to a Natural Womanhood article a couple of years ago which asked about the potential impact of cervical ectropion on charting. The quick summary is that most methods can accommodate the fluid signs and intermittent bleeding which can be seen with cervical ectropion. Fluid signs may be much more robust and could be prolonged, but in general women will still be able to clearly identify the difference between types of fluid secretions relative to ovulation.
So, just know that if you've been diagnosed with cervical ectropion it's likely something your NFP instructor has encountered before and can give you some strategies to navigate with your method! If, however, you do experience issues with fluid observations related to this condition, there are plenty of method options or additional biomarkers you could consider adding in, depending on your personal situation, goals, and preferences. So just be sure to speak with your instructor and your doctor about what might be the best options for YOU regarding treatment and ongoing management.
❤️ Loved this post? Be sure to subscribe to the Body Lit Library weekly newsletter, where every Thursday you'll get access to new content, updates, and special insider offers!
📚 Want to learn more? Check out our lifelong body literacy education courses and books, from puberty through perimenopause and everything in between: pearlandthistle.com


